
Hypertension is one of the major risk factors for kidney disease. What is most challenging is that it often shows no obvious symptoms in its early stages but may have already silently damaged the microvasculature of the kidneys. By the time proteinuria or a decline in eGFR appears, kidney function is often already deteriorating.
Hypertension Often Has No Symptoms in Early Stages
The Nursing Department of Taipei Veterans General Hospital points out: "Hypertension often has no noticeable symptoms in its early stages, and most patients are only diagnosed after organ function has been impaired." This is why hypertension is known as the "silent killer," as it can cause severe organ damage even without symptoms.
Blood Pressure Standards Are Closely Linked to Kidney Disease Risk
Hypertension is diagnosed when systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg, and treatment is recommended.
For patients with chronic kidney disease (CKD), proteinuria, diabetes, etc., the KDIGO 2021 and ACC/AHA 2017 guidelines recommend maintaining blood pressure below 130/80 mmHg. If proteinuria is present, further lowering SBP to <120 mmHg can help slow kidney function deterioration.
How Does Hypertension Harm the Kidneys?
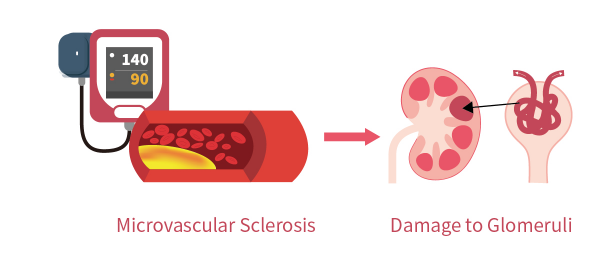
- Microvascular Sclerosis → Damage to Glomeruli
Prolonged hypertension leads to microvascular sclerosis and hyaline degeneration in the kidneys, impairing glomerular filtration function and reducing the efficiency of waste and water excretion.
- Proteinuria as an Early Warning Sign
The presence of proteinuria indicates that the glomeruli have already begun to sustain damage. KDIGO guidelines recommend prioritizing the use of ACEI/ARB medications in cases of proteinuria and controlling SBP to below 120 mmHg to help slow the progression of kidney disease. - Decline in eGFR Indicates Kidney Function Deterioration
When eGFR drops below <60 mL/min/1.73m², it signifies the onset of chronic kidney disease. Studies have shown that for every 10 mmHg increase in SBP, the annual decline rate of eGFR increases by approximately 0.2 mL/min/1.73m².
Why Is Hypertension Often "Unnoticeable" Yet High-Risk?
Most patients do not exhibit symptoms such as foamy urine, swelling, or fatigue in the early stages of kidney disease. It is often discovered during health checkups or when kidney function abnormalities are detected.
International guidelines such as KDIGO and ACC/AHA point out that even in the absence of symptoms, active intervention should be initiated if SBP ≥ 130 mmHg or DBP ≥ 80 mmHg to prevent kidney and cardiovascular damage.
Understanding Kidney Risk Through Data
|
Specific Protective Strategies
- Regular Blood Pressure Monitoring — Recommended at least once a week for individuals over 40, those with a family history, or those with metabolic syndrome.
- Annual Proteinuria and eGFR Checks — Can be done via urine and blood tests during health checkups or outpatient visits.
- Healthy Lifestyle: Daily salt intake <6g, at least 150 minutes of aerobic exercise per week, quitting smoking, limiting alcohol, and maintaining an ideal weight.
- Avoid Long-Term Use of NSAIDs — Prolonged use increases the risk of kidney damage.
Although early-stage hypertension often shows no obvious symptoms, it poses a hidden threat to kidney health. Only through regular monitoring and proactive health interventions can we protect kidney function and reduce the risk of chronic diseases.
References
[1]Taipei Veterans General Hospital - Care for Hypertensive Nephropathy
[3]Relationship Between Blood Pressure and Incident Chronic Kidney Disease in Hypertensive Patients Trends of Blood Pressure Control in Chronic Kidney Disease Among US Adults: Findings From NHANES 2011 to 2020
